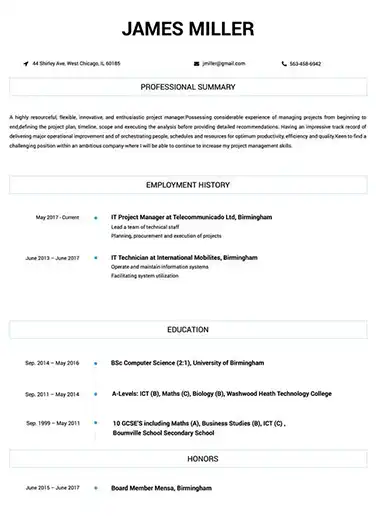
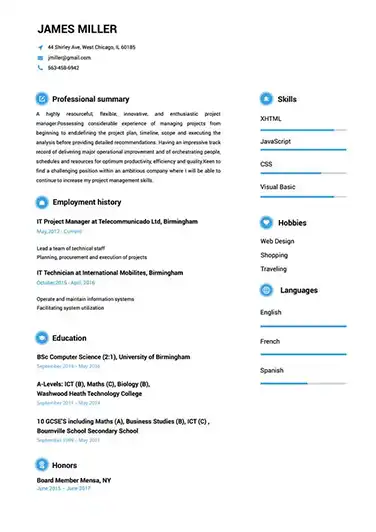
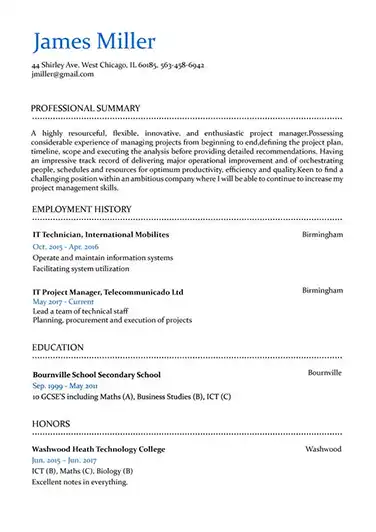
Use This Template
Use This Template
Build your resume in 15 minutes
Create an awesome resume that meets the expectations of potential employers with our selection of professional, field-tested resume templates.
medical billing specialist: Resume Samples & Writing Guide
gray_danny@outlook.com
659-051-6385
Professional Summary
Employment history
- Updating patient accounts
- Entering patient information into medical billing software
- Resolving insurance and billing discrepancies
- Updating patient accounts
- Processing payments
- Following up on unpaid claims
- Updating patient accounts
- Entering patient information into medical billing software
- Preparing invoices and statements
Education
Skills
Do you already have a resume? Use our PDF converter and edit your resume.
tayloradam@zoho.com
833-171-5916
Professional Summary
Employment history
- Processing payments
- Communicating with insurance companies
- Maintaining patient records
- Resolving insurance and billing discrepancies
- Auditing medical records for accuracy
- Resolving patient billing disputes
- Resolving patient billing disputes
- Verifying insurance coverage
- Answering patient and insurance inquiries
Education
Skills
jack.miller@outlook.com
995-266-6776
Professional Summary
Employment history
- Auditing medical records for accuracy
- Resolving patient billing disputes
- Processing payments
- Processing insurance claims
- Updating patient accounts
- Scheduling patient appointments
- Processing payments
- Auditing medical records for accuracy
- Updating patient accounts
Education
Skills
smith.william@inbox.com
782-974-2838
Employment history
- Maintaining patient records
- Verifying insurance coverage
- Preparing invoices and statements
- Processing insurance claims
- Processing payments
- Resolving patient billing disputes
- Answering patient and insurance inquiries
- Resolving insurance and billing discrepancies
- Processing insurance claims
Education
Skills
smith_gus@aol.com
763-709-2385
Employment history
- Verifying insurance coverage
- Preparing invoices and statements
- Auditing medical records for accuracy
Education
Skills
Not in love with this template? Browse our full library of resume templates
medical billing specialist Job Descriptions; Explained
If you're applying for an medical billing specialist position, it's important to tailor your resume to the specific job requirements in order to differentiate yourself from other candidates. Including accurate and relevant information that directly aligns with the job description can greatly increase your chances of securing an interview with potential employers.
When crafting your resume, be sure to use action verbs and a clear, concise format to highlight your relevant skills and experience. Remember, the job description is your first opportunity to make an impression on recruiters, so pay close attention to the details and make sure you're presenting yourself in the best possible light.
medical billing specialist
- Process medical charges and check filing claims.
- Interacted regularly with medical professionals regarding billing polices/procedures.
- Trained/coached new employees.
- Provide the solutions and suggestions on queries (floor assistance).
medical billing specialist
- Received and posted payments from clients and insurance companies.
- Worked with various insurance companies to resolve denied claims.
- Resolved billing issues identified by insurance carriers and patients.
- Reviewed claim denials and payer requirements for corrective action and prevention in the future.
- Researched and replied in a timely manner to insurance, patient, and internal customer inquiries.
- Researched and resolved denials and EOB rejections within standard billing cycle timeframe.
- Reviewed billing edits and provided insurance company with correct information.
senior medical billing specialist
- Maintaining Issue logs, Update tracker, Clarification log for the assigned Clients
- Weekly basis Web Ex interaction with US clients to discuss about process trends.
- Provide the training pertaining to the process as per the updates by the client.
- Preparing the SOP of the workflow for better understating of the process.
medical billing specialist
- Accurately posted/submitted claims for multiple offices.
- Researched CPT/ICD-9 coding discrepancies for compliance and reimbursement accuracy.
- Posted insurance payments/adjustments manually.
- Prepared daily deposits.
- Updated patient demographics/verified insurance eligibility.
- Covered various administrative positions throughout practice as needed.
medical billing specialist
- Handle Inbound and Outbound calls associated with inurance companies and patient inquiries.
- Accurately review accounts with patients according to their coordination of benefits and forwarding accounts for adjustments to ensure correct patient responsibility.
- Correspond with insurance companies for reprocessing of denied claims with HCPC codes, ICD-9 codes.
- Requesting back up documentation and uploading missing invoices for customers request.
- Billing Medicare and private insurance companies for DME supplies.
medical billing specialist Job Skills
For an medical billing specialist position, your job skills are a key factor in demonstrating your value to the company and showing recruiters that you're the ight fit for the role. It's important to be specific when highlighting your skills and ensure that they are directly aligned with the job requirements, as this can greatly improve your chances of being hired. By showcasing your relevant skills and experience, you can make a compelling case for why you're the best candidate for the job.
How to include technical skills in your resume:
Technical skills are a set of specialized abilities and knowledge required to perform a particular job
effectively. Some examples of technical skills are data analysis, project management, software proficiency,
and programming languages, to name a few.
Add the technical skills that will get hired in your career
field with our simple-to-use resume builder. Select your desired resume template, once you reach the skills
section of the builder, manually write in the skill or simply click on "Add more skills". This will
automatically generate the best skills for your career field, choose your skill level, and hit "Save &
Next."
- Data Entry
- Medical Terminology
- Coding
- Insurance Claims
- Medical Billing Software
- ICD-10
- HIPAA Compliance
- A/R Follow-up
- Reimbursement Procedures
- Accounts Receivable
- Microsoft Office
- Medical Records
- A/P Processing
- Electronic Medical Records
- Claim Denial Management
- Payment Posting
- CPT Coding
- Revenue Cycle Management
- Claims Processing
- Insurance Verification
- Healthcare Regulations
How to include soft skills in your resume:
Soft skills are non-technical skills that relate to how you work and that can be used in any job. Including
soft skills such as time management, creative thinking, teamwork, and conflict resolution demonstrate your
problem-solving abilities and show that you navigate challenges and changes in the workplace
efficiently.
Add competitive soft skills to make your resume stand-out to recruiters! Simply select
your preferred resume template in the skills section, enter the skills manually or use the "Add more skills"
option. Our resume builder will generate the most relevant soft skills for your career path. Choose your
proficiency level for each skill, and then click "Save & Next" to proceed to the next section.
- Communication
- Interpersonal
- Leadership
- Time Management
- Problem Solving
- Decision Making
- Critical Thinking
- Creativity
- Adaptability
- Teamwork
- Organization
- Planning
- Public Speaking
- Negotiation
- Conflict Resolution
- Research
- Analytical
- Attention to Detail
- Self-Motivation
- Stress Management
- Collaboration
- Coaching
- Mentoring
- Listening
- Networking
- Strategic Thinking
- Negotiation
- Emotional Intelligence
- Adaptability
- Flexibility
- Reliability
- Professionalism
- Computer Literacy
- Technical
- Data Analysis
- Project Management
- Customer Service
- Presentation
- Written Communication
- Social Media
- Troubleshooting
- Quality Assurance
- Collaboration
- Supervisory
- Risk Management
- Database Management
- Training
- Innovation
- Documentation
- Accounting
- Financial Management
- Visualization
- Reporting
- Business Acumen
- Process Improvement
- Documentation
- Relationship Management.
How to Improve Your medical billing specialist Resume
Navigating resume pitfalls can mean the difference between landing an interview or not. Missing job descriptions or unexplained work history gaps can cause recruiters to hesitate. Let's not even talk about the impact of bad grammar, and forgetting your contact info could leave your potential employer hanging. Aim to be comprehensive, concise, and accurate.
Employment history
- Resolving patient billing disputes
- Generating reports and analyzing data
- Entering patient information into medical billing software
- Resolving patient billing disputes
- Answering patient and insurance inquiries
- Processing payments
Education
Skills
Include your Contact Information and Job Descriptions
Missing job descriptions lessens your chances of getting hired.
Key Insights- Employers want to know what you've accomplished, so make sure to include descriptions for all of your previous jobs.
- Keep job descriptions short but don't just list your jobs.
- Never copy-paste a job description to post on your resume. Get inspired and use tools to help you write customized descriptions.
How to Optimize Your medical billing specialist Resume
Keep an eye out for these resume traps. Neglecting to detail your job roles or explain gaps in your career can lead to unnecessary doubts. Grammar blunders can reflect negatively on you, and without contact information, how can employers reach you? Be meticulous and complete.
adamsdanny@zoho.com
953-916-8964
Employment history
- Proccessing payments
- Communicating with insuarance companies
- Answering patiant and insuarance inquirys.
- Verifying insurance coverag,
- Maintaning patient records,
- Audting medical records for accuraccy.
- Maintaining patien't records
- Verifying insuranc'e coverage
- Auditing medical record's for accuracy
Education
Skills
Correct Grammar and Address Gap Years in Your Resume
Don't leave unexplained gaps in your work history.
Key Insights- When explaining gaps in your employment section, start by being honest.
- Elaborate on the gap and show that you never stopped learning.
- Explain and elaborate any gap in your work history by highlighting new skills.
medical billing specialist Cover Letter Example
A cover letter can be a valuable addition to your job application when applying for an medical billing specialist position. Cover letters provide a concise summary of your qualifications, skills, and experience, also it also gives you an opportunity to explain why you're the best fit for the job. Crafting a cover letter that showcases your relevant experience and enthusiasm for the Accounts Payable role can significantly improve your chances of securing an interview.
Gray gray_danny@outlook.com
659-051-6385
449 Cypress Avenue, Westhope, ND
58793
Microsoft
Redmond, Washington
To the Hiring Team at Microsoft
I am writing to express my interest in the Lead Medical Billing Specialist position at Microsoft. As a Medical Billing Specialist with 13 years of experience in Administrative & Clerical myself, I believe I have the necessary skills and expertise to excel in this role.
Growing up, I always had a fascination with Scheduling. As I pursued my education and gained experience in this field, I realized that this was where I could make the most impact. I have had the opportunity to work on things throughout my career like personal projects and voluntary work, which have developed in me a deep understanding of the challenges and opportunities in this field. I am excited to bring my passion and expertise to the role at and help your organization achieve its goals.
I am elated about the opportunity to join a team that shares my passion for this field, and values collaboration and innovation. I am confident that together we can overcome whatever tests and challenges are put on our way.
Looking forward to hearing from you,
Danny Gray
659-051-6385
gray_danny@outlook.com
Danny Gray
Showcase your most significant accomplishments and qualifications with this cover
letter.
Personalize this cover letter in just few minutes with our user-friendly tool!
Related Resumes & Cover Letters

Build your Resume in 15 minutes
Create an awesome resume that meets the expectations of potential employers with our selection of professional, field-tested resume templates.